Contact customer service

You are:
All standards of French and international learned societies have, for more than 10 years, recommended mouth care in intensive care, and more particularly with patients under mechanical ventilation
In France, whether it is the SFAR (French Society of Anesthesia Resuscitation) or the SRLF (French Society of Resuscitation in French), these two organizations have taken positions to promote oral care (1), or even oropharyngeal disinfection (2), as preventive measures in the occurrence of pneumonias acquired under mechanical ventilation.
Thus, it is now established that mouth care carried out at a frequency of 6 treatments per 24 hours presents one of the best preventions to fight against Acquired Pneumonia under Mechanical Ventilation (APMV). One of the primary sources of nosocomial infections in intensive care is these lung diseases. They participate in the increase of the average length of stay in intensive care and present a significant financial burden for these care units..
A review of the scientific literature, carried out by the Inter.med and Didactic teams, gathers the data which justify these elements; this technical-scientific file is available on simple request by activating the link appearing at the end of this article.
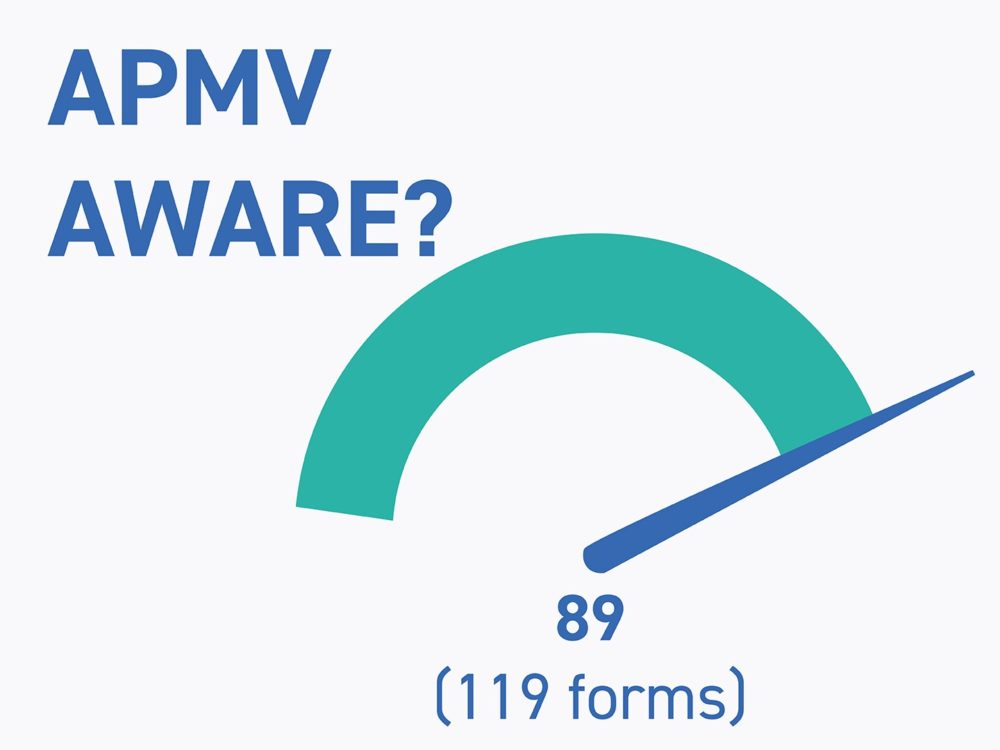
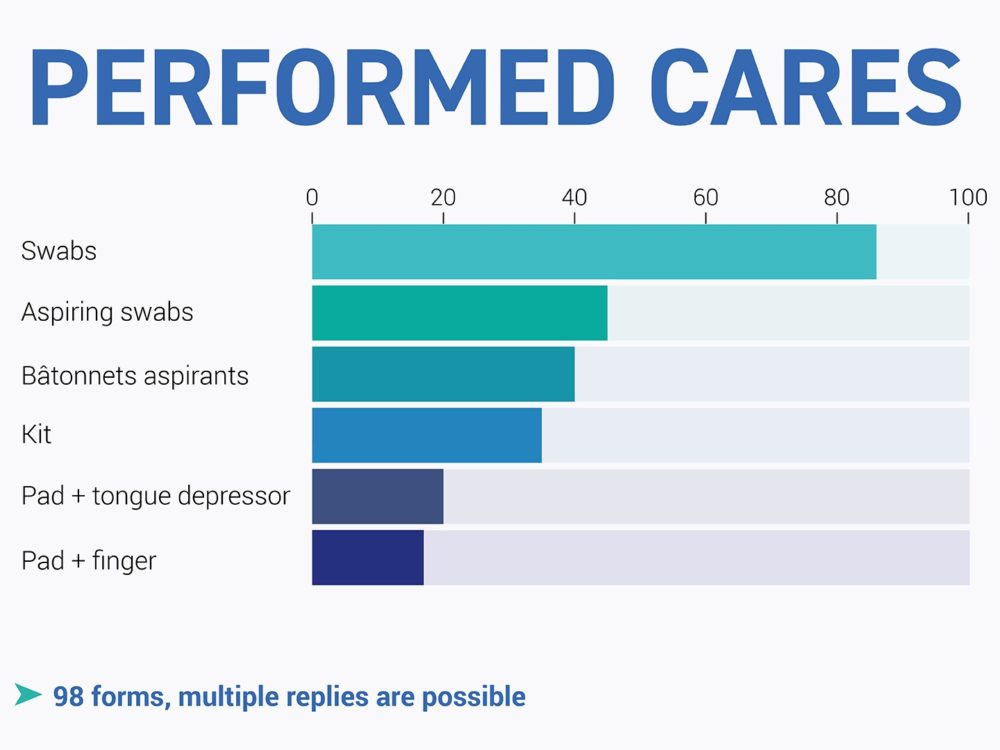
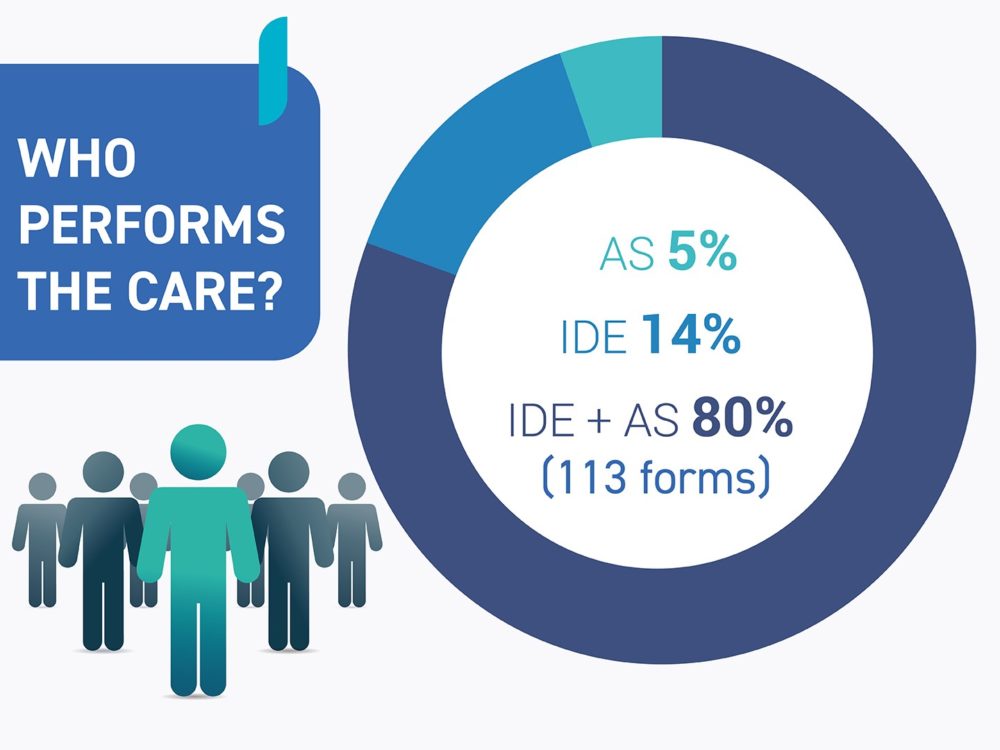
Inter.med Laboratoires carried out a field survey of intensive care units in the public and private sectors of at least ten intensive care beds. In most cases, these were versatile resuscitation units.
The following items were collected from around 120 healthcare facilities across the country.
In a number of testimonies, it was noted:

Inter.med Laboratoires, the French benchmark in the production of devices for mouth care, has therefore taken all these observations into account to offer healthcare teams very high quality devices, made in France, adapted to the daily practices of caregivers.
Also as part of the development of this range, Inter.med laboratories pays particular attention to the impact on hospital waste in order to reduce packaging waste as much as possible (polyethylene bag, cardboard and recyclable boxes.)
To receive our technical-scientific file, contact us